Bleomycin
View Brand InformationWhat is Bleomycin?
Approved To Treat
Related Clinical Trials
Summary: This phase III trial compares the effect of adding immunotherapy (brentuximab vedotin and nivolumab) to standard treatment (chemotherapy with or without radiation) to the standard treatment alone in improving survival in patients with stage I and II classical Hodgkin lymphoma. Brentuximab vedotin is in a class of medications called antibody-drug conjugates. It is made of a monoclonal antibody call...
Summary: This phase III trial studies how well active surveillance help doctors to monitor subjects with low risk germ cell tumors for recurrence after their tumor is removed. When the germ cell tumor has spread outside of the organ in which it developed, it is considered metastatic. Chemotherapy drugs, such as bleomycin, carboplatin, etoposide, and cisplatin, work in different ways to stop the growth of t...
Summary: RADAR is a multicentre, international, randomised, open-label phase III clinical trial composed of 2 trials running in parallel. Trial 1 will be led and sponsored by University College London (UCL) and conducted in Europe and Australia/New Zealand. Trial 2 will be led by the Canadian Cancer Trials Group (CCTG) and conducted in North America, with CCTG the regulatory sponsor in Canada, and Universi...
Related Latest Advances
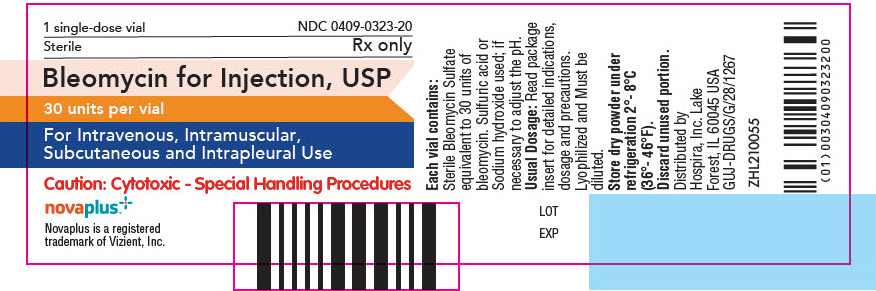
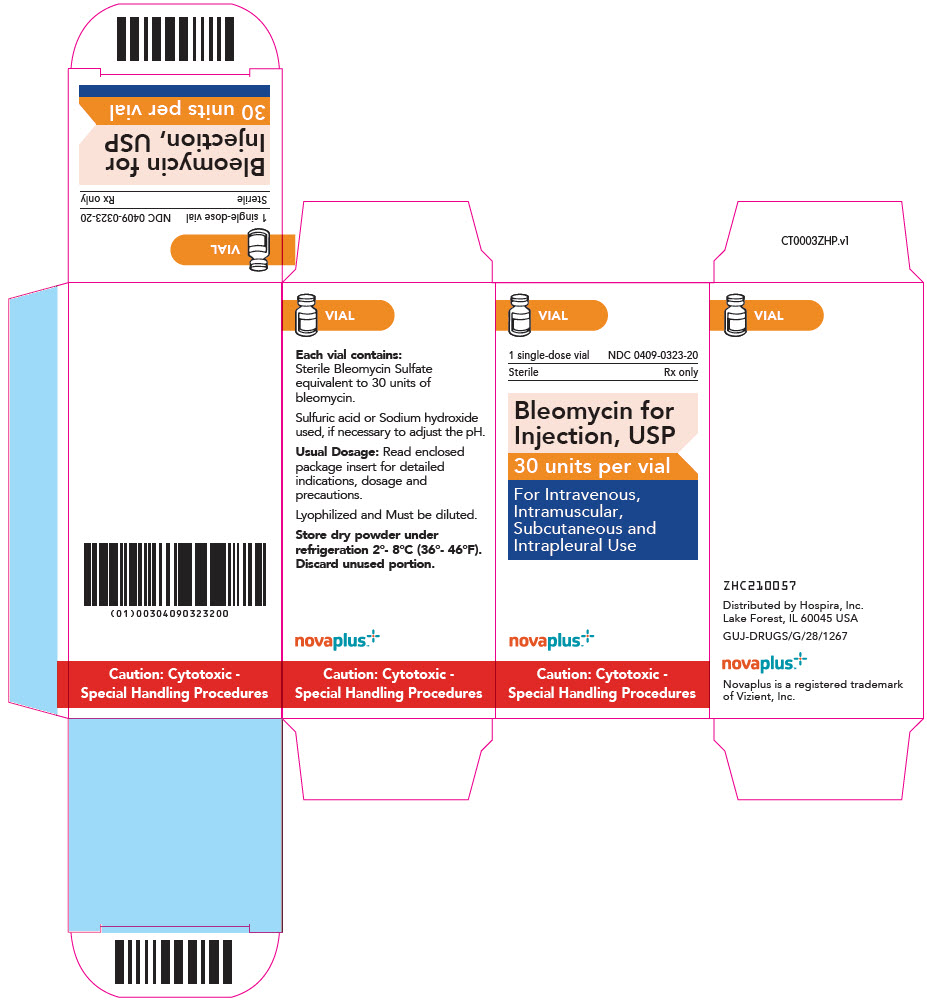
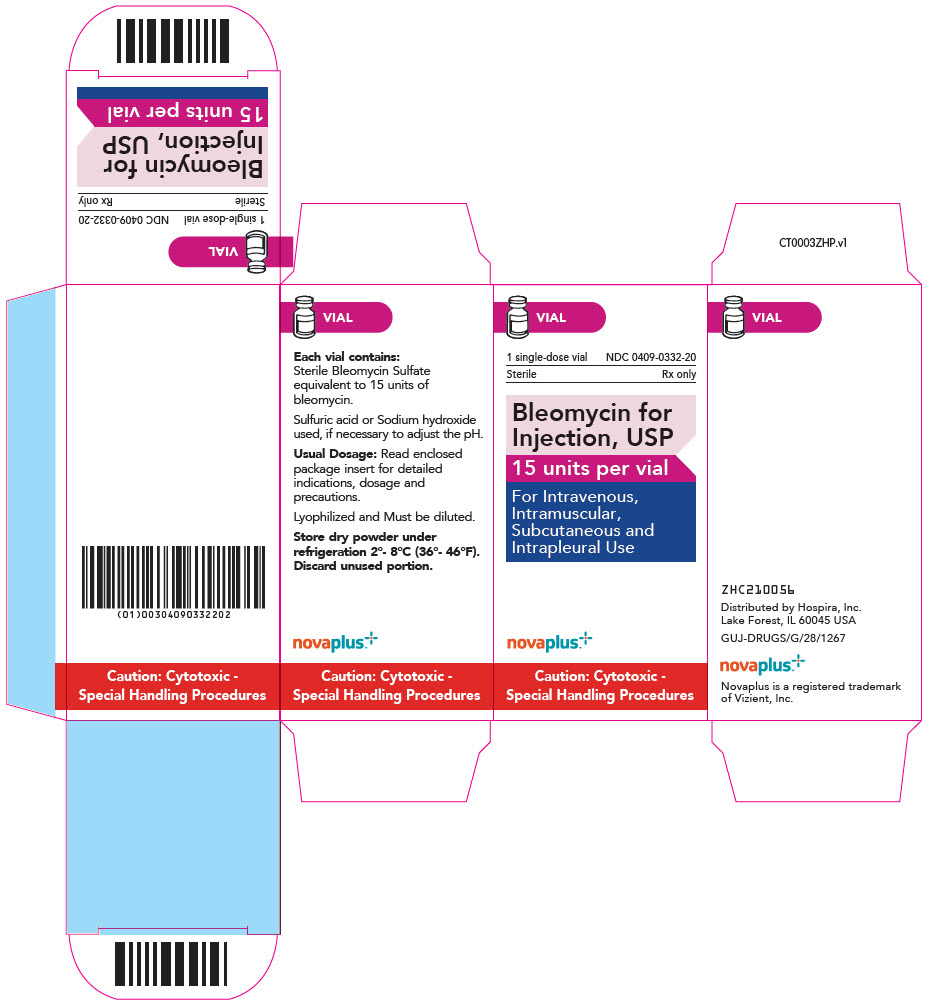
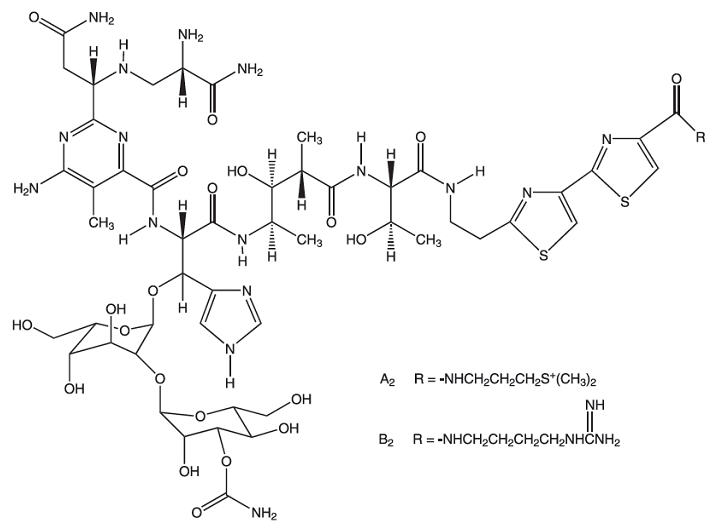
Brand Information
Bleomycin is effective as a sclerosing agent for the treatment of malignant pleural effusion and prevention of recurrent pleural effusions.
- CrCL can be estimated from the individual patient's measured serum creatinine (Scr) values using the Cockcroft and Gault formula:
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004 165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling occupational exposure to hazardous drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs.
- Polovich M, White JM, Kelleher LO, eds. 2005. Chemotherapy and biotherapy guidelines and recommendations for practice. 2nd ed. Pittsburgh, PA: Oncology Nursing Society.